Bimonthly assessment Decemberr
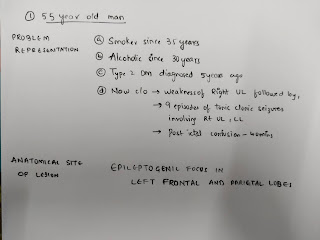
1) A 55 year old man with Recurrent Focal Seizures
Detailed patient case report here: http://ushaindurthi.
blogspot.com/2020/11/55-year- old-male-with-complaints-of. html 1. What is the problem representation of this patient and what could be the anatomical site of lesion ?
Reference
https://www.epilepsy.com/living-epilepsy/epilepsy-and/professional-health-care-providers/co-existing-disorders/brain-tumors-1
2. Why are subcortical internal capsular infarcts more common that cortical infarcts?
Lacunar syndromes are clinical manifestations of lacunar infarctions. Lacunar infarctions are defined as small subcortical lesions with a size of less than 15 mm in diameter caused by occlusion of a penetrating artery from a large cerebral artery, most commonly from the Circle of Willis. These penetrating arteries arise at sharp angles from major vessels and are thus, anatomically prone to constriction and occlusion.
https://www.ncbi.nlm.nih.gov/books/NBK534206/#:~:text=Lacunar%20syndromes%20are%20clinical%20manifestations,from%20the%20Circle%20of%20Willis
3. What is the pathogenesis involved in cerebral infarct related seizures?
There are several causes for early onset seizures after ischaemic strokes. An increase in intracellular Ca2+ and Na+ with a resultant lower threshold for depolarisation, glutamate excitotoxicity, hypoxia, metabolic dysfunction, global hypoperfusion, and hyperperfusion injury (particularly after carotid end arterectomy) have all been postulated as putative neurofunctional aetiologies. Seizures after haemorrhagic strokes are thought to be attributable to irritation caused by products of blood metabolism. The exact pathophysiology is unclear, but an associated ischaemic area secondary to haemorrhage is thought to play a part. Late onset seizures are associated with the persistent changes in neuronal excitability and gliotic scarring is most probably the underlying cause. Haemosiderin deposits are thought to cause irritability after a haemorrhagic stroke.14 In childhood, post‐stroke seizures can occur as part of perinatal birth trauma.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2585721/
Suggested model – Ischemic stroke leading to maladaptive plasticity and PSE: Following a cerebral vascular occlusion, thrombin increases in the brain. This increase may be as a result of BBB breakdown and entrance of vary blood components into the brain parenchyma or by brain tissue intrinsic production. Thrombin and its main receptor PAR1 enhance NMDA receptor activity and calcium entry, thus leading to a hyperexcitable state and to maladaptive plasticity. Eventually, synchronized epileptic activity occurs as a part of a PSE condition.
https://www.frontiersin.org/articles/10.3389/fncel.2019.00397/full
4. What is your take on the ecg? And do you agree with the treating team on starting the patient on Enoxaparin?
Ecg on day 28/11
ECG on day (28/11)
a.sinus tachycardia(HR:150),narrow qrs
b.ST depressions in anteroseptal leads(V1,v2,v3),but with no reciprocal changes:cant be considered NSTEMI
(NSTEMI is when there are no changes on ECG with elevated cardiac enzymes-trop I would have helped to confirm)
c.left axis deviation+
d.right bundle branch block
e.left ventricular hypertrophy+(R in aVl >12mm)
Ecg on Day 3/12:
Comments
COULD BE MALIGNANT VENTRICULAR PREMATURE COMPLEXES POST ACUTE MYOCARDIAL INFARCTION
http://hqmeded-ecg.blogspot.com/2018/10/anterior-stemi-and-multiform-pvcs-with.html?m=1
Yes.i accept treating team starting the patient on Enoxaparin in view of anteroseptal NSTEMI
The Recommendation:
The AHA and ACC guidelines state, “In patients with NSTE-ACS, anticoagulation, in addition to antiplatelet therapy, is recommended for all patients irrespective of initial treatment strategy. Treatment options include:
Enoxaparin: 1 mg/kg subcutaneous every 12 hours, continued for the duration of hospitalization or until PCI is performed. An initial IV loading dose is 30 mg (Level of evidence A)
Unfractionated heparin (UFH) IV: initial loading dose 60 IU/kg (max 4000 IU) plus 12 IU/kg/h (max 1000 IU/h) adjusted per activated PTT in according to specific hospital protocol (Level of evidence B)”[2]
Bivalirudin/Fondaparinux- These are other options outside the scope of this post
5. Which AED would you prefer?
According to the history after 9episodes of focal seizures there 2 episodes of GTCS after which he was brought to our hospital
Diagnosis POST STROKE PARTIAL SEIZURES WITH SECONDARY GENERALISTION
Please provide studies on efficacies of each of the treatment given to this patient.
1.Levetiractam and carbamezapine
The efficacy of LEV was found to be comparable to CBZ as monotherapy in the treatment of partial seizures. LEV did not show superior efficacy compared to CBZ. Both drugs equally reduced the seizure frequency compared to pretreatment seizure frequency. LEV was equally tolerable to CBZ. LEV and CBZ demonstrated equal incidence of AE. LEV can be safely used as monotherapy in the treatment of partial epilepsy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698781/
2.Atorvastatin
The SPARCL trial has shown that high dose atorvastatin is an effective medication for secondary prevention of stroke cardiovascular events in patients with no known history of cardiac disease
During the 4.9 years of follow-up in SPARCL, patients with recent stroke or TIA had a 5.1% incidence of a major coronary event (death from cardiac causes [1.6%], nonfatal myocardial infarction [3.5%]), major cardiovascular event (17.2%), any coronary event (8.6%) and need for revascularization (coronary, carotid or peripheral; 6.9%).7 High dose atorvastatin reduced major coronary events by 35% (HR 0.65,CI 95% 0.49–0.87), any coronary event by 42% (HR 0.58, 95% CI 0.46–0.73]) and the need for revascularization by 45% (HR 0.55, 95% CI 0.43–0.72).7
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2856578/#!po=55.9524
3.Ecospirin
Random allocation to long-term aspirin therapy reduced the risk of all serious vascular events by 13% (ie, stroke, myocardial infarction and vascular death; RR: 0.87%, 95% CI: 0.81 to 0.94).
https://www.ahajournals.org/doi/full/10.1161/strokeaha.107.497271#:~:text=26%E2%80%9336-,Efficacy,CI%3A%200.81%20to%200.94).
4.Enoxaparin
Enoxaparin was more effective than intravenous dose-adjusted UFH in reducing the incidence of the composite endpoint (including death, myocardial infarction or recurrent angina prompting urgent revascularization) in the majority of subgroups at 43 days after randomization.
https://pubmed.ncbi.nlm.nih.gov/11981102/#:~:text=Results%3A%20Enoxaparin%20was%20more%20effective,at%2043%20days%20after%20randomization.
5.Metformin and human mixtard :for blood sugar control
QUESTION 2
55 year old man with Recurrent hypoglycemia
Cause:IATROGENIC HYPOGLYCEMIA IN PATIENTS WITH RENAL INSUFFICIENCY (reduced excretion of hypoglycemic drugs causing hypoglycemic episodes)
Metformin. The only route of elimination of metformin is via the kidneys. Consequently it may accumulate in people with impaired renal function. Most guidelines recommend reviewing or reducing metformin dose when eGFR is <60 mL/min/1.73 m2
Sulfonylureas. Hypoglycemia risk is increased as a consequence of accumulation of the sulfonylurea and/or its active metabolites and their long duration of action
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4470208/#B65-jcm-04-00948
3. What is the cause for his Dyspnea? What is the reason for his albumin loss?
Cause of dyspnea :?heart failure,?B/L minimal pleural effusion secondary to hypoalbuminemia.
A 2D echo would help
Cause of albuminuria: DIABETIC nephropathy
A fundoscopy and USG abdomen for renal size and RPD changes would help
4. What is the pathogenesis involved in hypoglycemia ?
RISK FACTORS FOR HYPOGLYCEMIA IN DIABETES
The conventional risk factors are based on the premise that relative to low rates of glucose delivery into the circulation, high rates of glucose efflux out of the circulation, or both, or absolute therapeutic hyperinsulinemia is the sole determinant of risk (1, 2). They include:
- 1.
Insulin (or insulin secretagogue) doses are excessive, ill-timed or of the wrong type.
- 2.
Exogenous glucose delivery is decreased (as following missed meals and during the overnight fast, with gastroparesis or celiac disease).
- 3.
Glucose utilization and sensitivity to insulin are increased (as during and shortly after exercise, in the middle of the night, following weight loss or improved glycemic control).
- 4.
Endogenous glucose production is decreased (as following alcohol ingestion or in liver failure).
- 5.
Insulin clearance is decreased (as in renal failure).
https://www.ncbi.nlm.nih.gov/books/NBK279100/
5. Do you agree with the treating team on starting the patient on antibiotics? And why? Mention the efficacies for the treatment given?
Fever chart,CUE,urine cultures not available
No history of fever,No raised TLCs ,No consolidations on chest x ray
I dont agree with treating team starting antibiotics.
QUESTION 3
A. 41 year old man with Polyarthralgia
Case details here: https://
mahathireddybandari.blogspot. com/2020/11/41m-with-chest- pain-and-joint-pains.html?m=1 1. How would you evaluate further this patient with Polyarthralgia?
2. What is the pathogenesis involved in RA?
https://www.sciencedirect.com/science/article/pii/S1074761317300419
3. What are the treatment regimens for a patient with RA and their efficacies?
Drugs for rheumatoid arthritis
Treatment regimens of RA according to American college of rheumatology
Efficacy of drugs used for rheumatoid arthritis
The primary nonbiologic conventional disease-modifying anti-rheumatic drugs (DMARDs) include leflunomide, methotrexate, and sulfasalazine. Patients’ ability to remain on long-term therapy (ie, persistence) was improved with methotrexate compared with sulfasalazine.14 Methotrexate is considered the “anchor” DMARD, because of the extensive positive clinical and published experience accumulated with this agent.
Anakinra was less effective than etanercept with an odds ratio (OR) of 0.34 (95% confidence interval [CI], 0.14-0.81; P = .015) and adalimumab was more efficacious than anakinra (OR, 2.20; 95% CI, 1.01-4.75; P = .046).
A meta-analysis conducted by Aaltonen and colleagues recently examined tumor necrosis factor (TNF) inhibitors (eg, adalimumab, certolizumab, etanercept, golimumab, infliximab) with regard to efficacy and safety.17 The metaanalysis demonstrated that the overall ACR50 response to TNF inhibitor monotherapy at 6 months was greater than with placebo (risk ratio [RR], 4.07; 95% CI, 2.7-6.13), which was statistically improved relative to placebo by the individual agents adalimumab, etanercept, and certolizumab, but not infliximab or golimumab. Additionally, TNF inhibitor combination therapy with methotrexate was more effective than methotrexate alone (RR, 4.7; 95% CI, 3.07-7.19) or a TNF inhibitor alone (RR, 1.53; 95% CI, 1.08-2.17). Interestingly, high doses (relative to normal doses) of TNF inhibitors (infliximab, etanercept, adalimumab, golimumab, certolizumab) did not improve ACR50 (RR, 1.02; 95% CI, 0.9-1.15)
https://www.ajmc.com/view/ace006_12dec_gibofsky2_s303to14
B.
75 year old woman with post operative hepatitis following blood transfusion
Case details here: https://
bandaru17jyothsna.blogspot. com/2020/11/this-is-online-e- log-book-to-discuss.html 1.What are your differentials for this patient and how would you evaluate?
75year old female with post transfusion
a.hyperbilirubinemia
b.pancytopenia
c.hepatitis
d.fever
e.indirect coombs test positive
Rising total bilirubin,increased LdH,drop in hb,flank pain post transfusion,fever with chills a delayed transfusion reaction will be a differential
s/o hemolytic reaction following transfusion
EVALUATION
https://www.google.com/amp/s/slideplayer.com/amp/3882733/
2. What would be your treatment approach? Do you agree with the treatment provided by the treating team and why? What are their efficacies?
Supportive care is all that is needed,the treating team has provided adequate hydration and has given the required supportive care
4) 60 year woman with Uncontrolled sugars
http://manojkumar1008.
blogspot.com/2020/12/60-yr- old-female-with-uncontrolled. html 1. What is the problem representation of this patient?
Right upper lobe consolidation with Sepsis induced hyperglycemia2. What are the factors contributing to her uncontrolled blood sugars?
https://ebrary.net/27217/health/sepsis3. What are the chest xray findings?
Chest x ray taken in PA view,with no rotation,trachea shifted to right,right upper lobe opacity?consolidation,costophrenic angles normal,heart size and border normal ,no bony abnormalities, diaphragm normal.
4. What do you think is the cause for her hypoalbuminaemia? How would you approach it?
- Inflammation (acute phase reactant)
- Malnutrition
- Albuminuria (protein losing diabetic nephropathy)
5. Comment on the treatment given along with each of their efficacies with supportive evidence.
Piptaz & clarithromycin : for his right upper lobe pneumonic consolidation and sepsis
Egg white & protien powder : for hypoalbuminemia
Lactulose : for constipation
Actrapidpid / Mixtard : for hyperglycemia
Tramadol : for pain management
Pantop : to prevent gastritis
Zofer : to prevent vomitings
5) 56 year old man with Decompensated liver disease
Case report here: https://appalaaishwaryareddy.
blogspot.com/2020/11/56year- old-male-with-decompensated. html 1. What is the anatomical and pathological localization of the problem?
Liver : Chronic liver disease (cirrhosis) secondary to HBV
2. How do you approach and evaluate this patient with Hepatitis B?
https://www.researchgate.net/figure/Anti-viral-Therapy-Options-for-HBeAg-Positive-Chronic-Hepatitis-B-patients-CHB-Chronic_fig4_281442059
3. What is the pathogenesis of the illness due to Hepatitis B?
Attachment
The virus gains entry into the cell by binding to receptors on the surface of the cell and entering it by endocytosis mediated by either clathrin or caveolin-1.
Penetration
Following endocytosis, the virus membrane fuses with the host cell's membrane, releasing the nucleocapsid into the cytoplasm
Uncoating
Because the virus multiplies via RNA made by a host enzyme, the viral genomic DNA has to be transferred to the cell nucleus. It is thought the capsid is transported on the microtubules to the nuclear pore. The core proteins dissociate from the partially double stranded viral DNA, which is then made fully double stranded (by host DNA polymerases) and transformed into covalently closed circular DNA (cccDNA) that serves as a template for transcription of four viral mRNAs.
Replication
The largest mRNA, (which is longer than the viral genome), is used to make the new copies of the genome and to make the capsid core protein and the viral RNA-dependent-DNA-polymerase.
Assembly
These four viral transcripts undergo additional processing and go on to form progeny virions which are released from the cell or returned to the nucleus and re-cycled to produce even more copies.
Release
The long mRNA is then transported back to the cytoplasm where the virion P protein synthesizes DNA via its reverse transcriptase activity.
https://en.m.wikipedia.org/wiki/Hepatitis_B_virus
https://www.semanticscholar.org/paper/Pathogenesis-of-Hepatitis-B-Virus-(HBV)-Mediated-Lu/ea7e186bcc3d4fcf0ae65ee39dc32a461f1f152d4. Is it necessary to have a separate haemodialysis set up for hepatits B patients and why?
Yes , separate machines must be used for patients known to be infected with HBV (or at high risk of new HBV infection). A machine that has been used for patients infected with HBV can be used again for non-infected patients only after it has been decontaminated using a regime deemed effective against HBV because of increased risk of transmission due to contamination.5. What are the efficacies of each treatment given to this patient? Describe the efficacies with supportive RCT evidence.
- Lactulose : for prevention and treatment of hepatic encephalopathy. https://pubmed.ncbi.nlm.nih.gov/27089005/
- Tenofovir : for HBV
- Lasix : for fluid overload (AKI on CKD) https://www.ncbi.nlm.nih.gov/books/NBK499921/#:~:text=The%20Food%20and%20Drug%20Administration,failure%20including%20the%20nephrotic%20syndrome.
- Vitamin -k : for ? Deranged coagulation profile (PT , INR & APTT reports not available)
- Pantop : for gastritis
- Zofer : to prevent vomitings
- Monocef (ceftriaxone) : for AKI (? renal)
QUESTION 6
58 year old man with Dementia
Case report details: http://
jabeenahmed300.blogspot.com/ 2020/12/this-is-online-e-log- book-to-discuss.html 1. What is the problem representation of this patient?
58 year old man with Slurring of speech since 6 months
Drooling of saliva and food from the mouth since 6 months
Urinary incontinence since 6 months
Forgetfulness since 3 months
Dysphagia to both solids and liquids since 10 days
2. How would you evaluate further this patient with Dementia?
https://www.aafp.org/afp/2018/0315/p398.html3. Do you think his dementia could be explained by chronic infarcts?
Yes
Dementia is common after stroke but we know little of the mechanisms or whether the risk varies with stroke subtype.
Stroke risk factors, amounts and regions of the brain affected, and suggested stroke mechanisms all vary with stroke subtype, and could influence the risk of cognitive impairment after stroke. For example, as cortical ischaemic strokes often affect a large area of brain, they may carry a higher risk of cognitive impairment than the smaller, less neurologically severe, lacunar strokes. Alternatively, lacunar strokes may carry a higher risk of cognitive impairment than would be expected on the basis of the lacunar infarct alone as they are part of the spectrum of cerebral small vessel disease (SVD). SVD, which affects the brain diffusely and is the commonest vascular cause of cognitive impairment, could be unmasked by a new lacunar stroke.
https://jnnp.bmj.com/content/84/8/893
4. What is the likely pathogenesis of this patient's dementia?
5. Are you aware of pharmacological and non pharmacological interventions to treat such a patient and what are their known efficacies based on RCT evidence?
P - 974 Patients with probable or possible VaD were randomized 2:1 to receive donepezil 5 mg/d or placebo
I - Donepezil 5mg/d
C - Placebo
O - Patients with hippocampal atrophy who were treated with donepezil demonstrated stable cognition versus a decline in the placebo-treated group; in those without atrophy, cognition improved with donepezil versus relative stability with placebo.
Patients treated with donepezil 5 mg/d demonstrated significant improvement in cognitive, but not global, function.
https://pubmed.ncbi.nlm.nih.gov/20395618/
QUESTION 7
7) 22 year old man with seizures
Case report here http://geethagugloth.
blogspot.com/2020/12/a-22- year-old-with-seizures.html 1. What is the problem representation of this patient ? What is the anatomic and pathologic localization in view of the clinical and radiological findings?
22 year old man with complaints of headache since 2 months and involuntary stiffness of bilateral upper and lower limbs since 1 week along with Loss of consciousness.
Anatomical localisation - Brain
Involving both the upper limbs and lower limbs
Could be due to multiple infarcts
Ring enhancing lesions as he is RVD positive
Radiologically
Shows ring enhancing lesions
2. What the your differentials to his ring enhancing lesions?
Cerebral abscess
Tuberculoma
Neurocysticercosis
Metastasis
Glioblastoma
Subacute infarct/haemorrhage/contusion
Demyelination (incomplete ring)
Tumefactive demyelinating lesion (incomplete ring)
Radiation necrosis
Postoperative change
Lymphoma - in an immunocompromised patient
Leukaemia
Thrombosed aneurysm
Necrotising leukoencephalopathy after methotrexate
A helpful mnemonic is MAGIC DR
https://radiopaedia.org/articles/cerebral-ring-enhancing-lesions
3. What is "immune reconstitution inflammatory syndrome IRIS and how was this patient's treatment modified to avoid the possibility of his developing it?
A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy in HIV-infected patients is defined as immune reconstitution inflammatory syndrome.
Despite numerous descriptions of the manifestations of IRIS, its pathogenesis remains largely speculative. Current theories concerning the pathogenesis of the syndrome involve a combination of
1. Antigenic burden
2. degree of immune restoration following
3. Host genetic susceptibility.
https://www.mdpi.com/life/life-10-00262/article_deploy/html/images/life-10-00262-g001.png
Major criteria
Atypical presentation of “opportunistic infections (OI) or tumors” in patients responding to antiretroviral therapy.
Decrease in plasma HIV RNA level by at least 1 log10copies/mL.
Minor criteria
Increased blood CD4+ T-cell count after HAART.
Increase in immune response specific to the relevant pathogen, e.g. DTH response to mycobacterial antigens.
Spontaneous resolution of disease without specific antimicrobial therapy or tumor chemotherapy with continuation of antiretroviral therapy.
BHIVA has issued guidelines for starting the TB treatment with HAART. If CD4+ count is less than 100 cells/μl, both anti-tuberculosis drugs and HAART can be started together. If CD4+ cells are in the range of 100-200; HAART is started 2 months after starting TB treatment. If the CD4+ cells are above 200, HAART is started 6 months after completing TB treatment.
8) Please mention your individual learning experiences from this month.







































Comments
Post a Comment