Bimonthly assessment February
CASE 1
50 year man, he presented with the complaints of
Frequently walking into objects along with frequent falls since 1.5 years
Drooping of eyelids since 1.5 years
Involuntary movements of hands since 1.5 years
Talking to self since 1.5 years
More here: https://archanareddy07.blogspot.com/2021/02/50m-with-parkinsonism.html?m=1
Case presentation links:
https://youtu.be/kMrD662wRIQ
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation
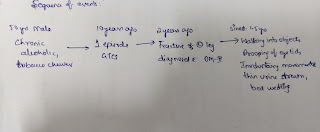
50 year man chronic alcoholic and tobbaco chewer with and previously with aggressive behaviour and history of GTCS 10years ago
History of fracture of left leg operated and was diagnosed to be diabetic 2 years ago,
Now presented with the complaints of
Frequently walking into objects along with frequent falls since, Drooping of eyelids(progressing as the day passes) and ,involuntary movements of hands ,Talking to self since 1.5 years . previously aggressive and now not expressing emotions,and also thin urine stream since 1year,chronic hypokalemia,
Anatomical location Basal ganglia
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
Sequence of events
Etiology
Reduced arm swing
Bradykinesia
Hypertonia
Upward gaze palsy
Negative ice pack test
H/o falls, emotional instability
Patients with Progressive supra nucelar palsy show a degeneration of neurons that occurs in the basal ganglia--the part of the brain that helps coordinate and ensure smooth body movements--and in the brain stem, the part of the brain that controls vital body functions (e.g., breathing, heart rate, swallowing) and eye movements. In addition, neurofibrillary tangles are detected (containing abnormal tau protein), and strokes (lacunar) may occur in the basal ganglia and deep white matte
https://www.uspharmacist.com/article/progressive-supranuclear-palsy
The patient fits well into the NIND criteria, after excluding the exclusion criteria.
c) What is the efficacy of each of the drugs listed in his current treatment plan
Tab SYNDOPA 110mg PO TID
PSP is an incurable condition. Treatment is supportive and far less effective than that for Parkinson's disease.The treatment of PSP remains unsatisfactory, since only occasionally do levodopa, dopamine agonists (TABLE 2), amantadine, or amitriptyline partially relieve rigidity. It is presumed that the reason PSP is not responsive to dopamine replacement or dopamine agonist therapies is that dopamine receptors are decreased as a result of postsynaptic damage beyond pathological changes seen in PD.Symptomatic treatment with drugs and other therapies should be targeted at reducing morbidity and improving quality of life (e.g., depression can be treated with selective serotonin reuptake inhibitors). Pharmacists should note that prior to initiating any treatment, the overall benefit-to-risk ratio to the individual patient must be considered.
Due to adverse effects associated with dopamine agonists--including nausea, hypotension, confusion, and hallucinations--their utility is severely limited.4 A recently published reassessment of risks and benefits of dopamine agonists in PD has revealed the occurrence of increasingly recognized adverse effects such as lower extremity edema, daytime somnolence, impulse control disorders, and fibrosis.
The antiviral agent amantadine was accidentally discovered to have an antiparkinsonism action (e.g., increasing release of dopamine among other effects).Adverse effects associated with amantadine therapy include restlessness, agitation, confusion, and hallucinations; high doses may result in an acute toxic psychosis.Peripheral edema, orthostatic hypotension, urinary retention, dry mouth, and livedo reticularis (i.e., red to blue skin discoloration on the limbs and trunk that intensifies upon exposure to cold) may also occur.
The geriatric patient population may be more susceptible to the central nervous system effects of amantadine; the use of two divided daily doses may minimize this effect.In patients with renal impairment, amantadine requires renal dosing based on estimated creatinine clearance. Monitoring parameters for amantadine therapy include renal function, Parkinson's symptoms, mental status, and blood pressure.
Nonpharmacologic measures introduced early in the course of disease may include weighted walking aids or wheelchairs to prevent falls, and adaptive eyeglasses (e.g., bifocals, prisms) to improve vision. Also important in the early stage of the illness is the introduction of physical therapy, occupational therapy, and speech therapy as supportive measures. Thus far, surgical approaches to PSP have proven ineffective.
A randomized, placebo-controlled trial in Germany looked at the short-term effects of coenzyme Q10 in PSP.Results indicated significant changes in the occipital lobe and a consistent trend in the basal ganglia.Coenzyme Q 10 treatment compared to placebo showed clinical improvement according to the PSP rating scale and the Frontal Assessment Battery; although the improvement was slight, it was noted as significant. The researchers concluded that since coenzyme Q 10 appears to improve cerebral energy metabolism in PSP, long-term treatment might have a disease-modifying, neuroprotective effect.
https://www.uspharmacist.com/article/progressive-supranuclear-palsy
CASE 2
2) Patient was apparently asymptomatic 2 years back then he developed weakness in the right upper and lower limb, loss of speech.
More here: https://ashfaqtaj098.blogspot.com/2021/02/60-year-old-male-patient-with-hrref.html?m=1
Case presentation links:
https://youtu.be/7rnTdy9ktQw
a). What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
problem representation:
progressive sob from grade 2 to 4 since 2 months
orthopnea,pnd
b/l pedal edema upto knee since 2 months
Generalised weakness since 2 months
H/o cva (rt hemiparesis recovered) with persistent loss of speech since 2 years.
anatomical localisation
based on history:pnd ,sob with orthopnea suggest left heart failure
based on examination:
shift of apex to 6th ics,presence of thrill palpable at apex(?s1), nature of the apex not mentioned
presence of loud p2 ,dilated veins ,pedal edema,s3 in both apical and left parasternal areas.
(?biventricular failure)
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
Etiology:
CAD
Ecg showing
1)normal axis
2)pathological Q waves from v1 to v6
3)poor R wave progression
suggest a CAD probably involving LAD and LCX territory
confirmed with finding on the echo leading to heart failure
c) What is the efficacy of each of the drugs listed in his current treatment plan
1)salt and fluid restriction
https://pubmed.ncbi.nlm.nih.gov/23787719/#:~:text=Conclusion%3A%20Individualized%20salt%20and%20fluid,Quality%20of%20life%3B%20Salt%20restriction.
Ninety-seven stable patients in NYHA class II-IV, on optimal medication, with previous signs of fluid retention, treated with either >40 mg (NYHA III-IV) or >80 mg (NYHA II-IV) of furosemide daily were randomized to either individualized salt and fluid restriction or information given by the nurse-led heart failure clinics, e.g. be aware not to drink too much and use salt with caution, and followed for 12 weeks. Fluid was restricted to 1.5 L and salt to 5 g daily, and individualized dietary advice and support was given.
Results After 12 weeks, significantly more patients in the intervention than in the control group improved on the composite endpoint (51% vs. 16%; P < 0.001), mostly owing to improved NYHA class and leg oedema. No negative effects were seen on thirst, appetite, or QoL
2)benfomet as thiamine replacement in alcoholic pts
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4550087/
3)aldactone(spironolactone)
https://www.aafp.org/afp/2001/1015/p1393.html
Based on earlier work suggesting a benefit of therapy,2 the Randomized Aldactone Evaluation Study (RALES) was undertaken to evaluate the role of spironolactone when used in addition to standard therapy for CHF. Standard therapy in this study did not include beta blockers
S-The investigators prospectively enrolled 1,663 patients with severe (New York Heart Association [NYHA] class IV) CHF (Table 1).4 Most of the enrolled patients were white men averaging 65 years of age. These patients had a left ventricular ejection fraction of 35 percent or less and marked physical limitations related to CHF. Patients were excluded if they had unstable angina or moderate renal failure, and if they were hyperkalemic.
All patients who could tolerate the drug were given an ACE inhibitor and a loop diuretic, and 70 percent were taking digoxin. Only 10 percent were taking beta blockers. Patients were randomly assigned to receive placebo or 25 mg of spironolactone daily in addition to their current regimen. After eight weeks, if the patient showed worsening CHF and had a stable potassium level, the dosage was increased to 50 mg daily. The dosage was decreased to 25 mg every other day if at any time the patient became hyperkalemic
4)furosemide 80mg
Diuretics are used to achieve and maintain euvolaemia (the patient’s ‘dry weight’) with the lowest possible dose. This means that the dose must be adjusted, particularly after restoration of the dry body weight, to avoid the risk of dehydration, which leads to hypotension and renal dysfunction.[10] It is important that treatment with diuretics is always coupled with neuro-hormonal system blocking, in order to slow down the progress of the disease.
In general, due to their greater effectiveness, loop diuretics, such as furosemide, are the mainstay of diuretic therapy in HF. Indeed loop diuretics produce more intense and shorter diuresis than thiazides, which results in more gentle and prolonged diuresis. They are, however, less effective in patients with reduced kidney function.[10] As a general rule, doses of loop diuretics should be as low as possible, in order to maintain a euvolaemic state. Restricting the amount of sodium and water, daily weight monitoring and avoidance of NSAIDs are critical in preventing salt and water retention.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6159465/
5)telmisartan 40mg
CASE 3
3) 52 year old male , shopkeeper by profession complains of SOB, cough ,decrease sleep and appetite since 10 days and developed severe hyponatremia soon after admission.
More here https://soumya9814.blogspot.com/2021/01/this-is-online-e-log-book-to-discuss.html?m=1
Case presentation video:
https://youtu.be/40OoVEQBgS4
a) What is the problem representation of this patient and what is the anatomical localization for his current problem based on the clinical findings?
Problem representation
52 year old male diabetic and hypertensive with complains of SOB, cough ,decrease sleep and appetite since 10 days .
Pure vegetarian with hb 5.7,macrocytes on smear suggesting Vit B12 deficiency and electrolyte imbalances
Anatomical location
sob without pedal edema, pnd, orthopnea can be localised to the lung
(sob on exertion grade 2 can also be localised the heart but no history or examination finding of pedal edema or jvp rise rules it out)
cough with sputum
b) What is the etiology of the current problem and how would you as a member of the treating team arrive at a diagnosis? Please chart out the sequence of events timeline between the manifestations of each of his problems and current outcomes.
ETIOLOGY
Anemia secondary to b12 Deficiency
?Sub acute combined degeneration of spinal cord secondary to vit B12 deficiency.
?Diabetic neuropathy
?Pseudohyponatremia secondary to uncontrolled sugars
? Hyponatremia secondary to SIADH due to penumonia
CAUSES OF Pseudo-hyponatremia (serum osmolality is normal or low)
Triglyceride level >1,500 mg/dL
High protein level (multiple myeloma, IVIG)
Profound hyperglycemia (DKA, Hyperglycemic Hyperosmolar Nonketotic Syndrome)
Exogenous osmoles:
Contrast dye
Mannitol administration
Maltose (from IVIG)
Sorbitol/glycine (used for surgical irrigation)
https://emcrit.org/ibcc/hyponatremia/
c) What is the efficacy of each of the drugs listed in his current treatment plan especially for his hyponatremia? What is the efficacy of Vaptans over placebo? Can one give both 3% sodium as well as vaptan to the same patient?
TREATMENT:
1.INJ.MONOCEF
Ceftriaxone therapy in otolaryngological and pulmonary infections:
The efficacy of ceftriaxone, 1 g given intramuscularly once daily, was evaluated in 38 patients with pneumonia (n = 11), pulmonary empyema (n = 2), bronchitis (n = 4), tonsillitis (n = 9), sinusitis (n = 7), and otitis (n = 5). Causative organisms were Streptococcus pneumoniae (n = 11), viridans type streptococcus (n = 1), Haemophilus influenzae (n = 6), group A streptococcus (n = 10), Staphylococcus aureus (n = 3), Klebsiella pneumoniae (n = 2), Pseudomonas aeruginosa (n = 1), Escherichia coli (n = 2), Proteus mirabilis (n = 1), and Proteus vulgaris (n = 1). Sterilization of infected foci was obtained in 89.4% of those treated, with clinical recovery in 86.8%. The ceftriaxone regimen was well tolerated.
https://pubmed.ncbi.nlm.nih.gov/3709268/
2.INJ.METROGYL
No justification found in the blog to start Metrogyl
3.INJ.OPTINEURON 1AMPULE IN1 NS /IV/OD
4.INJ.HAI S/C TID for control of sugars
5.T.TELMISARTAN
6.SYP.CITRALKA 5ML/PO/TID
7.SYP.ASCORYL
9.MONITOR VITALS
10.GRBS PROFILE (
7 POINT PROFILE ) MONITORING
VAPTANS
we shall discuss the role of vaptan treatment in chronic but not acute hyponatremia because the latter is rarely addressed in published literature.
THE INDICATIONS FOR VAPTANS ARE NOT CLEAR
1-First, we do not know how to distinguish between symptoms that are an indication for vaptan and those that are not.
2-Together, we lack information on which degree of severity of hyponatremia should give us reason to consider vaptan treatment.
3-Third, work by Gankam Kengne et al.28 suggested that patients with mild chronic hyponatremia fall to the ground more often than matched normonatremic controls .
We are unable to answer the question of whether elderly patients with chronic mild hyponatremia should be treated, for example, by a vaptan to correct hyponatremia and prevent fractures.
4-Fourth, in terms of indication for vaptan, the area least controversial might appear to be that of severe symptomatic (chronic) hyponatremia. A ‘hyponatremia-naive’ physician is likely to conclude that vaptans if anything should be promising in severe symptomatic hyponatremia. However, there are literally no published data on this. Clinical trials of vaptans have consistently excluded severe symptomatic hyponatremia from study because of ethical concerns (risk of worsening of severe symptoms when receiving placebo)
recent expert panel suggested that in severe symptomatic (chronic) hyponatremia, infusions of hypertonic saline should have priority over vaptan.30 This is an area of significant uncertainty. It has been pointed out that 3% NaCl may correct hyponatremia too quickly,31 or it may occasionally lead to pulmonary edema in SIAD(H). On the other hand, we have personal experience (PAG) that SIAD(H)-related severe symptomatic hyponatremia is a rewarding indication for vaptan. Thus, in the absence of a trial comparing fluid restriction plus 3% saline with vaptans in severe symptomatic hyponatremia, we do not have a database to make specific recommendations for or against vaptans.
https://www.sciencedirect.com/science/article/pii/S0085253815551089
4) Please mention your individual learning experiences from this month.
.Posted in department of nephrology
.Seen various cases of
CKD on medical management
CKD on MHD
Acute kidny injury and
Cardiorenal syndromes
.learnt about Approach to a patient with renal disease
.Learnt about the indications of dialysis
.I have put 5femoral vein and 3IJV catheters(learnt about the procedure)
.Learnt about management of electrolyte imbalances in pt s with CKD
.







Comments
Post a Comment