CLINICAL NEUROLOGY: THEORY TO PRACTICE-Teaching course
“CLINICAL NEUROLOGY”
“THEORY TO PRACTICE”
A well-organized teaching course in neurology was designed by me with the help of my fellow senior residents (Dr. Shashikala, Dr. Manasa, Dr. Pradeep, Dr. Vamshi, Dr. Manoj, Dr. Gouthami) with the support of our beloved HOD, Dr. Rakesh Biswas.
The main aim of this teaching course is to create interest among postgraduates in learning and teaching aspects of neurology. I planned to teach them on how to convert theoretical knowledge in neurology into practice.
I organized the course in such a way that each theory/seminar topic is followed by a relevant case presentation and journal. Postgraduates are trained in the theoretical aspects of the topic in the first class, and in the second class, the main focus is on examination techniques, making differential diagnoses, how to order appropriate investigations, and discussions on the management plan. Attendance to these sessions is monitored.
Each seminar will be followed by a short 'best of four MCQ' exam to check the level of understanding of post-graduates and also to generate a competitive spirit among the students.
During the seminar presentations as a course mentor, i go through the presentation of the post-graduate a day before and make necessary changes. As the presentation goes on, i try to simplify few complex concepts. I also check understanding among listeners from time to time.
During case presentations, the post-graduate presenting the case will be assessed for his/her history taking and examination skills. This will be followed by a discussion on investigations and formulating management plan.
All the post-graduates were asked to come prepared with the topic, at-least the basic aspects.
TOPIC- Arterial supply of brain and localization of stroke
PRESENTOR-Dr.Prachetan
MODERATOR-Dr.Chandana
19 post-graduate students have attended the seminar
Arterial supply was discussed under the following headings-
Posterior circulation
Territorial supply of brain(Lateral surface, medial surface, undersurface)
Anatomical course and branches of ICA,MCA,ACA,Circle of willis, PCA, Vertebro-basilar system.
Localization of stroke was discussed under the following headings-
ICA occlusion (Importance of ophthalmic artery,Angle brow and cheek pulsations, retinal changes)
ACA stroke- mechanism of mono-paresis based on motor homonculus and a brief discussion on mechanism of transcortical aphasias.
MCA stroke-Stem occulsion, M1 syndrome,M2 syndromes were dealt in detail with some example clinical scenarios given by me. Difference in clinical manifestations of involvement of dominant vs non-dominant hemisphere was explained.
Dominant-Language dysfunction, apraxias and angular gyrus(Grestmann syndrome),mechanism of alexia with agraphia was explained
Non dominant- Visuospatial neglect (explained with examples), dressing and constructional apraxias, emotional disturbances and delirium.
PCA strokes have been dealt in detail as P1 and P2 syndromes
P1- Dejerine-roussy syndrome,Thalamic syndromes
P2- Mechanism of various clinical manifestations have been dealt in detail such as-Visual agnosias, optic ataxia, balints syndrome, antons syndrome, asimultagnosia, pallinopsia, medial temporal lesions. Mechanism of alexia without agraphia was also explained by me.
Brain stem syndromes- Various named brain stem syndromes have been introduced and few of them were dealt in detail (Ventral mid brain syndromes, Millard gubler syndrome and lateral medullary syndrome).
A “best of four MCQ” exam was conducted after the session.
*Seminar 1 exam results 👏
*Highest score: 8/10*
Shiva kumar
Sree teja
Ajay
Govardhini
Navya
Prachetan
*2nd highest: 7/10*
Himaja
Vivek
Deepika
Kranthi
Venkat sai
Hari priya
Narsimha
Other post-graduates scored less than 7 were personally enquired about the problems and feedback was taken to improve the teaching sessions.
ASSESSMENT RESULTS OF FIRST YEAR POST-GRADUATES
FEEDBACK FORM-Out of 19, 9 post-graduates have answered questions in the feedback form.
Apart from session related feedbacks 2 interesting anonymous negative feedbacks have been found. Those feedbacks were related to the amount of stress he/she is facing when he/she has to manage the patient care, night duties and academics all together. As a result the academics seemed to be overburdening for them. My Plan is to address these concerns individually with counselling on how to manage the stress.
Reassurance was given in the 2nd session and a stress free and friendly environment rather than a formal teaching was promised to my students as far as my teaching sessions were concerned. I tried to engage each and every student in the room during the session. This change increased the amount of collective learning that has happened in the 2nd session and also few post-graduates asked doubts after the session which did not happen in the first session. Importance of creating a student friendly environment during the teaching sessions was the ultimate learning point for me.
CASE PRESENTATION
Presenter: Dr.Shiva Nagendra.
Moderator: Dr.Chandana
A total of 15 post-graduates attended the session.
69 year old female presented with sudden onset weakness of left upper and lower limb for 6 days with acute infarct in right fronto-parietal region with multiple hypertensive micro-haemorrhages
During the case presentation the post-graduate was assessed for history taking skills and examination skills.
Few mistakes have been identified and rectified
Technique for Examination of the fundus was explained to all the post-graduates.
Different clinical scenarios were given and final year pgs were questioned about the steps of management. Each step in the management was discussed seperately. A detailed lecture was given on each step of management according to guidelines.For example-
1.A case of acute stroke in window period(<4.5hrs)-Clinical assessment,NIHSS score,BP control,GRBS,CT+/-Angio, ASPECTS score, check list for thrombolysis, thrombolysis with alteplase, post thrombolysis monitoring, complications, and when to do repeat imaging were explained in detail by me.
2.A wake up stroke-Detailed explanation about diffusion-flair mismatch was explained with the help of MRI images.
3.A case of acute stroke outside the window period-Role of dual anti-platelet therapy and indications were discussed. Dosages of the drugs were discussed. Role of statins was discussed.
Followed by a brief lecture by me, on various scoring systems-
NIHSS score
ASPECTS score with example
Modified rankin scale
ABCD2 score in TIA
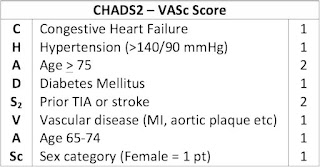
CHADS2VASc score in cardio-embolic strokes
HASBLED score for bleeding risk
Discussion on MRI -
how to differentiate T1,T2, Flair-with images.
Early changes of stroke in MRI-loss of grey white differentiation with example images.
Diffusion-Flair mismatch-with images
Difficult scenario such as infarct with bleed, clopidogrel vs ticagrelor, differentiation of TIA from early presentation of acute stroke were some of the inconclusive and controversial topics raised during the discussion. Post-graduates were encouraged to review the literature about them.
——————————-
APPROACH TO LMN
Number of pg’s attended-20
Approach to lower motor neuron diseases.
Students were given a basic orientation and recap of brachial plexus and lumbosacral plexus anatomy. Various dermatomes,myotomes,nerve supply of different muscle groups and action of different muscles at various joints were discussed .
LUMBOSACRAL PLEXUS

Each pg was given a clinical scenario to approach and localise the lesion. Each and every pg in the class was engaged.
The case scenarios were designed by me, based on my previous clinical experience and the cases that i have come across.
Take home points:
Step-1: upper motor neuron or lower motor neuron?
Step2: lower motor neuron, is it pure motor or motor-sensory or pure sensory?
Pure motor syndrome: Anterior horn cell, muscle or neuromuscular junction
AHC-Asymmetrical weakness with wasting more than weakness and fasciculation
Neuromuscular junction-Symmetrical proximal weakness with early EOM involvement with fatiguability and fluctuation suggests neuromuscular junction disease.
Muscle-Pure motor proximal weakness without fatiguability and fluctuation suggest muscle disease and Preserved reflexes.
If motor-sensory syndrome-Root,plexus or peripheral nerves, based on the distribution of motor weakness and sensory loss.
•Root-Radicular pain,dermatomal distribution,myotomal distribution
•Plexus-weakness and sensory loss in distribution of multiple peripheral nerve
•Nerve-mono neuropathy/polyneuropathy* usually sensorimotor but can be pure sensory or pure motor
Pure sensory-Ganglionopathies
Difficult to differentiate:
Multiple radiculopathy vs plexopathy vs multiple peripheral nerve palsies
POST SEMINAR ASSESSMENT RESULTS:
Highest-9/10
Sr.Venkat sai 👏
8/10👏
Dr.Govardhini
Dr.Ajay
Dr.Himaja
Dr.Kranthi
7/10👏
Dr.Narsimha
Dr.Nagendra
Dr.Lohith
_________________________________________--
CASE PRESENTATION
A Case presentation by Dr. Sree Teja
Moderator: Dr. Chandana
Attendance-19
Case:51 year old female with tingling and numbness of all 4 limbs for the last 6 months with burning paraesthesia of boot feet. She is a known diabetic with drug incompliance.
Dr. Sree teja was assessed on her skills on examination of the sensory system, mistakes were identified and knowledge gap was filled with further discussion and hands on experience of sensory system examination techniques.
Take home points:
Primary sensory modalities and methods of examination
-Touch,pain ,Temperature
-Joint motion
-position sense
-Rombergs
-Pseudoathetosis
Secondary sensory modalities and methods to examine
-Two point discrimination
-Tactile localization
-Tactile extinction or double simultaneous stimulation
Graphesthesia
Stereognosis
Peripheral neuropathy-Describe under 7 headings
1.Symmetrical or Assymetrical
2.Distal or proximal or both distal and proximal
3.Small fibre or large fibre neuropathy
4.Acute /sub acute/chronic/relapsing remitting
5.Axonal vs demyelination
6.Mononeuropathy vs polyneuropathy vs Mononeuritis multiplex
7.Likely etiology(Metabolic,infections,inflammatory,hereditary,Nutritional,Vascular,Compressive,Toxins)
Discussion on nerve conduction studies-basic mechanism and findings-
Reduced CMAP,SNAP in axonal neuropathy
Reduced conduction velocity and increased latency in demyelination
____________________________________________________________________
SEMINAR
Topic-Approach to headache
12post graduates attended the session
Before going into the details the need for headache as a topic for seminar comes from my experience where, one day i noticed a patient labelled with a diagnosis of migraine just because she has photophobia with some mild headache. Few patients are given a diagnosis of tension type headache instead of probable TTH even if the patient is not fitting into the criteria of TTH. This made me realise that there needs to be a session on IHS classification criteria for headache to build awareness on headache among post-graduates.
Presenting pg-Dr.Lohith varma
Moderator-Dr.Chandana
The session started with discussion about basic pain sensitive structures in brain (both extra and intra cranial)
Few cases were made up based on IHS criteria.
Each student was allotted a case of headache.History and examination details were given and the students were asked to diagnose the case.
After assessing their answers I understood where the exact knowledge gaps are!
I explained them about the diagnostic criteria of different headaches according to IHS.
I started with ‘probable migraine’ (as these patients are commonly mislabelled as migraine)
Followed by diagnostic criteria’s of different headache cases was discussed.
A total of 11 cases followed by discussion was done
1. 2cases of probable migraine
2. Migraine without aura
3. Migraine with aura
4. Chronic migraine
5. Status Migrainous
6. Infrequent episodic tension type headache
7. Probable cluster headache vs cluster headache
8. Probable paroxysmal hemicrania vs Paroxysmal hemicrania
9.Short lasting neuralgiform headache attacks-SUNCT vs SUNA
10. Hemicrania continua
Each case was followed by discussion on diagnostic criteria.
Other primary headaches were explained briefly.
After filling the knowledge gaps in the topic of primary headaches , we came to the classification of secondary headaches.
Importance of numerical allotted to each secondary headache in IHS criteria was discussed with appropriate examples.
Dr.Lohith gave a brief presentation on management of all primary headaches with particular focus on first line drugs for each headache, acute management vs prophylaxis
Importance of Indomethacin responsive headaches such as paroxysmal hemicrania and Hemicrania continua, was emphasised
Post session exam was conducted with 4 easy to answer questions,3 questions which were moderately difficult,3 questions which are difficult to answer based on the opinion of Senior residents.
9/10👏
Dr.Venkat sai
7/10👏
Dr.Lohith
Dr.Shiva kumar
Dr.Deepika
I appreciate nagendra also👏he is the only person who answered last question correctly (question based on difference between SUNCT and SUNA)
Post session exam key was released in our chat group and followed by a text quoted below to keep them going
“ Cross check your answers.
This is just to help you learn some points and build a competitive spirit among you guys.
Even if you get fewer marks, there's nothing to worry about. Just make sure your knowledge is better than yesterday.
Always keep learning new things.”
Getting more marks is not the agenda of these exams. These MCQs are designed in a format that makes post-graduates think and exercise their minds with the aim to solve them. I hope eventually it becomes a habit and they incorporate this into their real-world clinical practice.
___________________________________________________________________________-
CASE PRESENTATION-
Presenter- Dr. Akash
Moderator-Dr. Chandana
The session started with case presentation by Dr. Akash. The patient was a middle aged man with electric shock like pain sensation in trigeminal distribution ,each attack lasting 2-3mins , occurring several times a day. Patient also had conjunctival redness and lacrimation.
Differentials after the case presentation were,
-Trigeminal neuralgia
-Short lasting neuralgiform headaches
Dr.Akash was assessed on his history taking skills for a of headache
Importance of the following in case of headache was emphasised,
1.Age
2.Onset-
A case scenario of severe acute headache with sub-arachnoid haemorrhage was given as example.
3.Region/Location of headache
Bilateral forehead-TTH
Unilateral, fronto-parietal-Migraine
Unilateral, orbital, supra-orbital, temporal-TACs
Maxillary, mandibular with or without ophthalmic division regions in trigeminal neuralgia.
4.Radiation to neck-Meningitis
5.Characters of pain
Throbbing, Pulsating-Migraine
Dull, pressure like-TTH
Stabbing-TACs
Electric shock like-Trigeminal neuralgia
Worst headache ever/ thunderclap headache-SAH
6.Frequency in terms of how many times in a day? How many attacks in a month /year?
How much time is each attack lasting?
7.Red flag signs of headache were discussed
8.A example case scenario was given. Old aged male patient with proximal muscle weakness with temporal region pain and vision loss. Students identified it as GCA but failed to identify the associated polymyalgia rheumatica
9.Importance of other associated symptoms was discussed. Few of them are mentioned below,
Aura-Visual, Sensory, motor, retinal, speech, brain stem aura
Photophobia, phonophobia, osmophobia (sensitivity to light, sounds, and movements respectively) are features of migraine.
Limb weakness
Visual disturbance
Fever, neck stiffness. photophobia, and rash suggest meningitis
Scalp tenderness and jaw claudication are indicative of giant cell arteritis,
Cranial autonomic symptoms were discussed
Ear, tooth, facial, and neck pain are causes of referred pain to the head.
Nausea and vomiting are symptoms of migraine and elevated intracranial pressure.
Constitutional symptoms: weight loss and anorexia suggesting. neoplastic disease, fever
10.Variour precipitants of headache
11. Aggrevating and relieving factors were discussed
12. Important questions to ask in family and personal history was explained in detail.
Students were explained about the importance of stress factors in headache. The students were advised to take history related to stress under 4 headings not to miss anything.
WORK STRESS
FAMILY STRESS
FINANCIAL STRESS
PSYCHOLOGICAL STRESS
13.Various medications and their relation to headache was discussed, for example,
Analgesics-Medication overuse headache
Nitrates ,CCBs
Anticoagulant,antiplatelets-ICH
Steroids, OCPs, Vitamin A, Tetracylines-IIH
14.Dr.Akash was questioned on the further evaluation and management.
Further discussion was on types of trigeminal neuralgias which are,
Classical TN-Due to vascular compression
Secondary TN-Due to Space occupying lesions, Demyelination etc with deficits in sensory and motor components of trigeminal nerve
Idiopathic TN-No cause.
15.Importance of treatment resistant TN and MRI was discussed.
MRI FIESTA sequence was a new term introduced to the students and they were encouraged to review the literature on this topic.
16.Treatment was discussed as
First line drugs-Carbamazepine, oxcarbazepine along with dosages, side effects, and monitoring was discussed
Second line drugs-Gabapentin,pregabalin, phenytoin
A brief discussion on alcohol block of mandibular and mental nerves followed by a discussion on Microvascular decompression in cases with vascular compression
Radiofrequency thermocoagulation in old age patients
______________________________________________________________________________
SEMINAR ON SEIZURE SEMIOLOGY
Presenter: Dr. HIMAJA
Moderator: Dr. CHANDANA
18 post graduates attended the session
To begin the discussion, postgraduates were asked if they can localize a seizure focus based on clinical history. Many post-graduates are unaware about seizure semiology and localization of seizure focus. They are always trained in stroke localization but seizure localization is something which is often overlooked and that needs a meticulous history taking.
The discussion started with various signs and symptoms associated with seizures under the following headings:
1.Aura
2.Automatisms
3.Motor manifestations such as posturing (figure of 4 posturing)
4.Eye manifestations: versive and non-versive eye movements
5.Language disturbances
6.Ictal and post ictal phenomenon
ILAE 2017 classification of seizures was discussed and various changes that have been compared to previous ILAE classification were discussed
Each post-graduate was given a clinical scenario, where in the post-graduate tried localizing the seizure focus based on the semiology and they were assessed on their localizing skills.
After the exercise the discussion continued on,
1.Features of seizures with frontal lobe as a epileptogenic focus
2.Features of seizures with temporal lobe as a epileptogenic focus
3.Features of seizures with parietal lobe as a epileptogenic focus
4.Features of seizures with occipital lobe as a epileptogenic focus
Generalized seizure semiology was discussed: GTCS,Generalized absence seizure,Generalized myoclonic seizure ,atonic seizure.
Post-session assessment with 10mcqs was conducted with main focus on lobar localization of seizure and ILAE 2017 classification of seizure.
RESULTS:
Highest 10/10 👏💥💥💥
Dr.Bharath
Dr.Lohith
2nd highest 9/10 👏
Dr.Vivek
3rd highest 8/10 👏
Dr.Narsimha
Dr.Deepika
Dr.Hari priya
Dr.Ajay
------------------------------------------------------
CASE PRESENTATION
By Dr.Venkanna
A case of 30 year old male with left focal to bilateral tonic clonic seizure secondary to NCC, young onset HTN and HTN heart disease.
Dr. Venkanna was assessed on his history taking skills and examination skills
He missed the most important psychosocial aspects of the history
Post-graduates were asked to taken history from a patient with seizure in an organized way as stated below
1.History about the event:Age of onset, first episode or not, duration of each episode, time interval between each episode
2.Before the event:
Prodromal symptoms
Precipitants
Aura
Automatisms
3.During the eveng
Loss of consciousness
limb movements
posturing
eye and head movements
tongue bite, frothing, urine and fecal incontinence
Jacksonian march
4.After the event:
Post-ictal confusion
Limb weakness
Injuries
Time to full recovery
Speech arrest and behavior arrest
Recollection of events
5.To rule out non epileptic attacks/Psychological causes
Atypical limb movements
retained awareness during the event
vocalizations and response to commands during the attack
rapid recovery with no post-ictal confusion
atypical injuries
The discussion was followed by how to obtain relevant past medical history and drug history
Psychosocial stress factors were discussed.
Various causes of seizures were discussed under following headings:
-Neoplastic
-Vascular
-Trauma
-Metabolic
-Epileptic syndrome
Management in terms of which drug to start and when to start was discussed
various anti epileptics available and their mechanism of action was discussed
Newer drugs in epilepsy were given importance during the discussion
____________________________________________________________________
SESSION-9
SEMINAR-
TOPIC: NEURO-INFECTIONS
Presenter: Dr. VIVEK
Moderator: Dr. CHANDANA
Discussion on
1.Meningitis
2.Brain abscess
3.Encephalitis
1.Meningitis
Each post-graduate was given a case of meningitis along with CSF findings to solve.
a. Bacterial meningitis b. Viral meningitis c. Fungal meningitis d. Tubercular meningitis
The post-graduates easily diagnosed bacterial meningitis but most of them got confused in differentiating viral meningitis and tubercular meningitis as both have lymphocyte predominance in CSF.
This question solving exercise was followed by detailed discussion on the clinical presentation, CSF analysis and interpretation of CSF results to diagnose meningitis
Discussion on management of each type of meningitis .
Many post-graduates seem to be unaware that enterovirus are the most common causative agent for viral meningitis and needs only supportive care rather than acyclovir. Indications of acyclovir in viral meningitis was explained in detail.
Case scenario of HIV patient with meningitis was given and importance of having cryptococcal meningitis as differential was emphasized.
2.Brain abscess
Clinical presentation was discussed
MRI images were displayed and each post-graduate was asked to give one differential for ring enhancing lesion.
This was followed by discussion on ring enhancing lesions
Management of brain abscess was discussed.
3. Encephalitis
HSV encephalitis, Dengue and COVID encephalitis was discussed briefly
Differences between meningitis and encephalitis were discussed.
POST-SEMINAR assessment results (10 mcqs)
Highest 9/10
Dr. Nagendra
Dr. Vivek
Dr. Narsimha
Dr. Hari priya
2nd highest 8/10
Dr. Manohith
Dr. Deepika
Dr. Nishitha
Dr. Venkat sai
3rd Highest 7/10
Dr. Ajay
Dr. Lohith
Dr. Shiva kumar
Dr. Vyshnavi
_____________________________________________________________________
CASE PRESENTATION
By Dr. Ravi
MODERATOR: DR.CHANDANA
Link to the case report: 60 year male with HIV + TBM + Acute stroke +? Myeloneuropathy
The trainee was assessed for his history taking and examination skills with particular focus on how to elicit motor, cranial nerves examination and meningeal signs
Neurological manifestations in HIV were discussed in detail under the following headings:
1.Manifestations due to direct injury of HIV virus:
Sensory neuropathy- distal symmetric polyneuropathy, AIDP, CIDP
Vacuolar myelopathy
HAND-HIV associated neurocognitive disorders
2.Neuro-Infections in HIV:
Aseptic meningitis, Acute meningitis, HAND
Bacterial infections: Tuberculosis as TBM, Tuberculomas and Syphilis
Viral infections: Progressive multifocal leukoencephalopathy due to JC virus, HSV encephalitis, CMV encephalitis
Fungal infections: Cryptococcal meningitis
Protozoal infections: Cerebral toxoplasmosis
Each and every manifestation was briefly discussed.
3.CNS malignancies: Primary CNS lymphoma
4.Unmasking of Autoimmune diseases in HIV was discussed: Polymyositis, myaesthenia gravis, AIDP, multiple sclerosis.
5.Immune reconstitution syndrome in relation to the case presented was discussed.
____________________________________________________________
SEMINAR
TOPIC:
SPINAL CORD ANATOMY
APPROACH TO SPINAL CORD DISORDERS
NEUROGENIC BLADDER
_______________________________________________________________
Attendance-7 post-graduates
CASE PRESENTATION OF MYELOPATHY-Transverse myelitis
Discussion on localization of spinal cord pathology
ASSESSMENT WITH 10 MCQs ON SPINAL CORD LOCALIZATION
Results of assessment on spinal cord disorders
👏👏
1st -Lohith (10/10)
2nd-Tushara (9/10) and pavani (9/10)
3rd-Bharath(8/10) and prachetha(8/10)
__________________________________
SESSION-13
Lobar organisation and functions-
Subdivisions and functions of frontal lobe, parietal lobe, temporal lobe and occipital lobe are discussed
Lobar function tests-
FRONTAL LOBE-tests discussed were:
1. Wisconsin Card Sorting Test (WCST)
2. Stroop Test
3. Trail Making Test (TMT)
4. Verbal Fluency Tests
5. Digit Span Test
6. Controlled Oral Word Association Test (COWAT)
7. Rey-Osterrieth Complex Figure Test
8. Clock Drawing Test
9. Go/No-Go Task
10. Iowa Gambling Task
11.Motor luria, graphic luria, proverb interpretation, FAB
TEMPORAL LOBE Tests discussed were:
Auditory Processing and Language Comprehension
a. Token Test
b. Boston Naming Test (BNT)
c. Wernicke’s Aphasia Assessment
2. Memory Function
a. Wechsler Memory Scale (WMS)
b. Rey Auditory Verbal Learning Test (RAVLT)
c. California Verbal Learning Test (CVLT)
3. Visual and Object Recognition
a. Benton Visual Retention Test
b. Facial Recognition Test
4. Temporal Lobe Epilepsy Assessment
a. EEG (Electroencephalogram)
PARIETAL LOBE;
1. Tactile Perception and Sensory Integration-Two-Point Discrimination Test, Stereognosis Test.
2.Visuospatial and Constructional Abilities: Rey-Osterrieth Complex Figure Test, Block Design Test, Clock Drawing Test.
3.Spatial Orientation and Awareness-Line Bisection Test, Cancellation Tests.
4.Mathematical and Calculation Skills- Calculation Tests.
5.Body Awareness and Somatosensory Integration: Finger Agnosia Test, Left-Right Orientation Test.
6.Praxis and Motor Coordination-Apraxia Tests(ideomotor apraxia)
OCCIPITAL LOBE:
1.Visual Acuity and Field Tests
- Snellen Chart
- Automated Perimetry
2.Color Perception
- Ishihara Color Test
3.Object and Face Recognition
- Visual Object and Space Perception (VOSP) Battery
- Benton Facial Recognition Test
4.Visual Integration and Processing
- Rey-Osterrieth Complex Figure Test
- Hooper Visual Organization Test
5.Motion Perception
- Kinetic Perimetry
6.Visual Attention
- Trail Making Test (Part A)
- Visual Search and Attention Test
Assessment results:
assessment on lobar function tests results
👏👏👏
1st- Bharath, venkat sai, nagendra, shiva kumar , narsimha, nishitha (8/10)
2nd-Hari priya ,pavani, prachethan (7/10)
____________________________________
LOBAR DYSFUNCTION-CASE PRESENTATION
A case presentation-Progressive supraneuclear palsy
Presentor: Dr.Tushara, Discussion by: Dr. Chandana.
History taking and examination of extra-pyramidal system was discussed in detail


































Comments
Post a Comment